Liver Disease and ICD-10
Liver disease is categorized in two ways by ICD-10: hepatic fibrosis and cirrhosis. ICD-10-AM is the Australian version of the 10th revision of the International Classification of Diseases. It is a classification system that allows doctors to describe the cause of a patient’s symptoms and diagnose the condition.
ICD-10-AM codes for cirrhosis
To improve detection rates of cirrhosis, ICD-10-AM codes were developed. These codes identify a subset of key complications of cirrhosis, including HCC, ascites, varices, SBP, and HE. They also help identify admitted episodes of care among patients with known cirrhosis.
This study examined 116 encounters deemed ‘liver-related’, including elective day admissions. Algorithm #1 correctly identified 75.9% of these encounters, whereas algorithms #1 and #6 correctly identified 92.3% and 100% of them, respectively. The algorithms also identified one-third of elective day admissions, including upper endoscopy and paracentesis. Of these, thirty-six percent of encounters were coded with an ICD-10-AM code.
These ICD-10-AM codes for cirrosis in liver disease are similar to those used in the parent classification. However, they lack codes for hepatic encephalopathy and spontaneous bacterial peritonitis. Despite the linguistic similarities between the two classifications, the Australian Modification (AM) codes for cirrhosis in liver disorder are significantly different from their American counterparts.
Although liver damage cannot be reversed, treatments for cirrhosis include medication and a positive lifestyle. Liver transplantation is usually a last resort. To claim the most appropriate reimbursement, medical billing and coding service providers can provide help. They will ensure that you submit the most accurate claims possible for reimbursement.
A number of complications of liver cirrhosis include high blood pressure in the veins, swelling of the legs and abdomen, blood clots, and infections. The disease also increases the risk of liver cancer. If you are diagnosed with cirrhosis, you should seek treatment immediately.
Patients with cirrhosis in the early stages may not exhibit any symptoms. A detailed medical history is necessary to identify the condition. The doctor may ask about your exposure to hepatitis C, alcohol use, or autoimmune diseases. A routine blood test can detect cirrhosis, but more advanced stages of the disease may require imaging and diagnostic tests.
When examining a patient with cirrhosis, it is essential to consider its severity and type. Cirrhosis may lead to severe scarring in the liver, which affects its capacity to function. Several factors may lead to the disease, including chronic alcohol use.
Impact of CLivD score on risk of liver disease
The impact of a high CLivD score on liver disease is still unclear. Some studies have shown that patients with COVID-19 have poorer outcomes than those without the disease. However, this association is not conclusive, and there is no nationwide data available from well-phenotyped cohorts with liver histology or matched general population controls.
A study conducted in Australia analyzed the impact of a high CLivD score on risk of liver diseases in a population-based cohort of 42,320 patients with biopsy-confirmed CLD. It included matched population controls, as well as matched patients with and without cirrhosis. The results were robust after sensitivity analyses and propensity score matching for significant comorbidities. Even when adjusting for age, cirrhosis-related comorbidity, and education level, the risk of COVID-19 was not predictive of overall mortality in the study population.
Regardless of the cause, chronic liver disease is characterized by progressive destruction of the liver parenchyma over time. It can be caused by a variety of conditions, including alcoholic liver disease, nonalcoholic fatty liver disease, and chronic viral hepatitis. Genetic, autoimmune, and viral factors can also play a role. A high score of CLivD is a risk factor for developing liver disease and higher rates of mortality.
A higher CLivD score also means more severe liver disease. Severe COVID-19 increases the risk of developing cirrhosis. In addition to liver disease, it is also a risk factor for hepatitis. It is essential to determine the severity of the condition before undergoing treatment.
The impact of CLD on risk of liver disease was studied using the Swedish healthcare registers, a nationwide database that included more confirmed cases of CLD than any previous study. This data allows researchers to calculate both absolute and relative risks more accurately. However, the study has many limitations.
In patients with CLD, the risk of death was more than double that of those with non-CLD. The results of Wu and Yang showed that patients with higher scores had a higher risk of developing severe liver disease compared to those without CLD. A similar finding was seen in two recent reviews by Sharma and Yadav et al. The authors also found a higher risk for severe liver disease in patients with CLD, who were previously hospitalized for liver disease, or had elevated levels of liver enzymes.
Impact of hepatic fibrosis on risk of liver disease
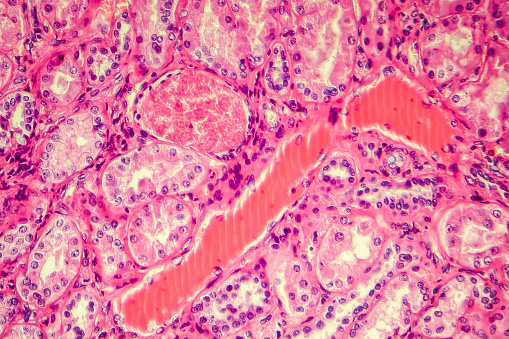
The impact of hepatic fibrosis (HF) on the risk of liver disease is complex. Fibrosis is a condition in which collagen and extracellular matrix proteins accumulate in the liver, causing scarring. It may develop over time and progress to more advanced stages. The rate at which fibrosis progresses varies, but some patients may develop cirrhosis within a few decades.
Hepatic fibrosis is an inflammatory condition of the liver that develops when hepatocytes are damaged. Inflammation causes repair cells to deposit collagen, which stiffens the liver tissue. This process continues unless the underlying cause is controlled. If chronic inflammation is not resolved, fibrosis progresses to cirrhosis.
The study aimed to clarify the role of hepatic fibrosis in metachronous liver-specific recurrence in colorectal cancer patients. While HF and NASH are closely related, the impact of HF on the risk of liver metastasis in CRC remains unclear.
HF has been associated with a poor prognosis for patients with colorectal cancer, suggesting that it may be a significant factor in the development of colorectal cancer. HF has also been associated with increased risk of liver metastasis.
DM has also been linked to the development of NAFLD and steatohepatitis. Overweight and obesity are risk factors for fibrosis. In combination, DM and obesity increase the risk of steatosis and cirrhosis.
Hepatic fibrosis has also been linked to the development of hepatic cancer. In one study, researchers found that chronic ethanol consumption of more than 40 grams a day was linked to increased risk of cirrhosis of the liver. The risk of hepatic fibrosis depends on various ethanol-mediated mechanisms, including alcoholic steatosis, and genetics.
While there are no definitive tests for identifying fibrosis, a common blood test, AST-to-platelet ratio (APRI), can determine whether or not someone has fibrosis. This test utilizes data from routine laboratory tests to determine a person’s risk of fibrosis.