Is Degenerative Disc Disease Hereditary?
There’s a lot of debate over whether or not degenerative disc disease is hereditary. A recent study by the University of Utah claimed that there is a genetic component to the disease, but this does not mean you’re predisposed to suffer from more disc issues or more pain. Nevertheless, there is a growing body of research that suggests that pain susceptibility is inherited.
At what age does degenerative disc disease begin?
Degenerative disc disease begins when discs lose their flexibility. This condition can lead to pain, degenerative scoliosis, and reduced mobility. The process has four stages: dehydration, disc dysfunction, stabilization, and collapse. The symptoms and treatments of each stage differ.
Disc degeneration can begin at an early age. A condition known as juvenile disc disorder, or juvenile discogenic disorder, affects people in their late teens and early 20s. While the exact cause is unclear, some physicians say that genetics is a large contributor. Others point to wear and tear on the body as the main culprit.
The symptoms of degenerative disc disease can range from a nagging pain in the back and neck to extreme pain in the legs and arms. Disc pain can also affect the nerves near the spine. If you experience any of these symptoms, you should schedule an appointment with a medical professional to determine if you have this condition.
What back problems are hereditary?
There are a few spinal conditions that run in families. The causes of these conditions are different in each family, but they usually relate to a person’s immune system or the functioning of the spine. One condition that has been found to run in families is scoliosis.
This degeneration is caused by heavy workloads and genetics is a major contributing factor. Research shows that as much as sixty to eighty percent of people with LDD have a genetic link to this condition. The findings show that LDD is influenced by genes, particularly ones related to peripheral structures, such as the spine and the brain. Genetic variation in genes related to nociceptive processing, tissue degeneration, and inflammation may be associated with a greater risk of developing back pain.
Some people have a higher risk of developing herniated discs than others. The same holds for degenerative disc disease, with people with an immediate family member experiencing disc-related lower back pain four times more likely to experience the condition. People with similar occupations and activities also have a higher risk of developing disc disease.
Can you stop degenerative disc disease?
Degenerative disc disease is a common affliction that affects your spine. This disease affects the shock-absorbing cushion between the adjacent vertebrae, which can eventually lead to arthritis and spinal stenosis. Although there is no cure for the disease, there are some lifestyle changes that may slow the progression.
Exercise can help your body recover faster from painful degenerative disc disease. A physical therapist can teach you how to properly lift weights and exercise the back. They can also teach you new movements to stretch your muscles and spinal discs. Stretching the back muscles will help relieve pain and increase flexibility. Physical therapy and pain medication can also help manage your condition.
Degenerative disc disease is a common cause of back pain, which can lead to disability. Discs are made of collagen and gelatinous material that breaks down with age. While this process is normal and can cause pain, some people can slow its progression and even reverse it.
What are the 4 stages of degenerative disc disease?
Degenerative disc disease is a degenerative disease that leads to several symptoms. In the early stages, people may have minimal symptoms. However, as the disease progresses, they will start to experience increasingly painful symptoms. These symptoms may include difficulty moving, muscle aches, and stiffness. If left untreated, this condition can result in severe back pain and disability. To avoid this, you should seek treatment as soon as possible.
The first stage is the stabilization phase, during which the spine tries to stabilize itself. However, this does not solve the problem. Over time, spinal discs begin to degenerate and the spinal bones begin grinding against each other, leading to bone spurs and inflammation.
What is L4-L5 degenerative disc disease?
The degenerative changes that occur in the L4-L5 disc are accompanied by pain in the legs. In addition, patients may experience numbness or tingling in the legs. For some patients, bowel or bladder control may also be affected. If left untreated, the condition can lead to paralysis of the legs.
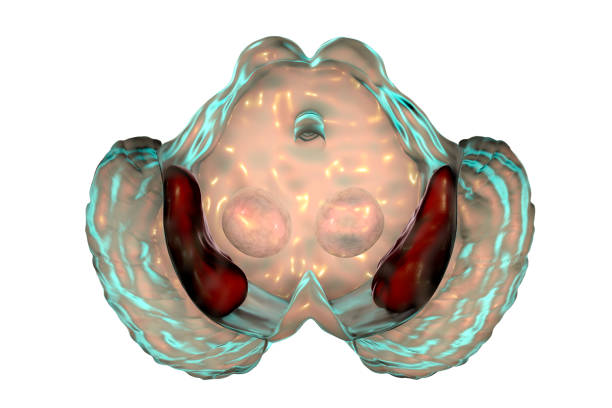
The L4-L5 disc is located between the two lowest vertebrae in the lumbar spine. It is at high risk of degeneration, because of the stress placed on it by the motion segment below the L4-L5 level. It can contain up to 80 percent water, which functions as a shock absorber. However, the loss of this water can result in less flexibility and pressure on the outer layer of the disc.
Patients with lumbar stenosis and disc herniation are at higher risk for developing this degenerative disc disease. This condition is typically associated with laxity of the ligaments and capsules of the L4-L5 disc space. It is also associated with degeneration of the facet joints.